The Systemic Shift: Pilates for the Menopausal Body
The conversation around menopause is finally changing. For too long, this biological transition was viewed through a narrow lens. We often focused solely on reproductive symptoms. However, as movement professionals, we must recognise menopause as a “systemic, total body event”. It impacts nearly every cell and system in the female body. This transition can begin as early as a woman’s 30s or 40s. Therefore, the majority of our clientele likely falls into the pre-, peri-, or post-menopausal demographic.
We must evolve our teaching strategies. We cannot simply rely on the same repertoire we used twenty years ago. We must integrate current science into our practice. At Polestar, we believe in meeting the client where they are. For the menopausal woman, this means understanding the profound physiological changes occurring beneath the surface.
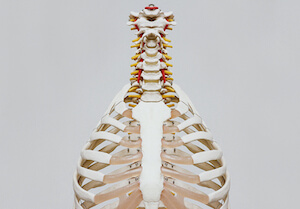
The Neuro-Endocrine Impact on Musculoskeletal Health
The decline in hormones is not just about mood or temperature regulation. The drop in oestrogen and progesterone dramatically alters musculoskeletal health. Oestrogen is vital for muscle proliferation. It is also crucial for blood supply. When oestrogen declines, muscle tissue tends to atrophy. This condition is known as sarcopenia.
This hormonal shift makes it significantly more difficult for women to build muscle. Furthermore, bone density takes a sharp downturn. Women can lose between 10% and 15% of their bone mass during the perimenopause transition alone. This is a critical window for intervention.
We also see metabolic changes. Oestrogen acts as an “elixir” for metabolic health. It helps transport glucose from the blood into the muscle. As oestrogen levels drop, this efficiency decreases. This can lead to insulin resistance and visceral fat storage. It also contributes to conditions like hyperlipidaemia or high cholesterol.
You may see clients who are “tired but wired”. This state of constant sympathetic drive disrupts sleep and recovery. Sleep is essential for neuroplasticity and tissue repair. Without it, the body cannot adapt to the physical demands we place upon it. We must view these symptoms as interconnected. A frozen shoulder may not just be an orthopaedic issue. It is often a symptom of menopause. New onset vertigo or joint pain may also be red flags.
Evidence-Based Movement Strategies
We must apply critical reasoning to our programming. We cannot use a “one size fits all” approach. The Polestar principles of movement science guide us here. We look at load, alignment, and mobility.
1. Graded Load and Joint Protection
Joint pain is a common complaint during menopause. This is often due to systemic inflammation. Pilates is uniquely suited to address this. We can use the equipment to provide assistance. We can offload the joints while still stimulating the muscles. This allows the client to move without fear or pain.
We must create positive movement experiences. If a client is in pain, we do not stop moving. We modify. We find a pain-free range of motion. We use the springs to support the weight of the limbs. This helps dampen the sensitised nervous system. It builds confidence and self-efficacy
2. Bone Health and Contraindications
We must be vigilant about bone health. A client may look fit but have low bone density. One case study revealed a 55-year-old woman with osteopenia who suffered a pelvic fracture from a simple fall. This highlights the silent nature of bone loss.
If a client has osteopenia or osteoporosis, we must adjust our repertoire. We must avoid loaded spinal flexion. Exercises like the Roll Over or Short Spine may be contraindicated. These movements place excessive compressive force on the anterior vertebral bodies. This increases the risk of compression fractures.
Instead, we focus on axial elongation. We strengthen the back extensors. We improve thoracic mobility to reduce load on the lumbar spine. We teach hip dissociation to spare the spine during daily tasks. This is the essence of pathokinesiology. We understand the pathology, and we adjust the mechanics accordingly.
3. The Necessity of Heavy Resistance
Pilates is an incredible tool. However, it may not be enough on its own for this population. The latest research suggests we need heavy resistance training. We need to stimulate the bone and muscle with significant load. Dr. Stacy Sims emphasises that women are not small men. We have different physiological needs.
The Pelvic Floor: Elasticity over Rigidity
Menopause also affects the pelvic tissues. The decline in oestrogen leads to dryness and thinning of tissues. This can affect the urethra and the vagina. It can lead to urinary incontinence or pelvic organ prolapse.
The old advice was simply to “strengthen” the pelvic floor. We now know this is insufficient. A healthy pelvic floor must be elastic. It must be able to contract and relax. It needs to respond to intra-abdominal pressure.
Many women hold tension in their abdominal wall and pelvic floor. This creates a hypertonic state. The muscles are tight but weak. They cannot respond to the load of a sneeze or a jump.
We must teach diaphragmatic breathing. The diaphragm and pelvic floor work in synergy. When we inhale, the pelvic floor should yield. When we exhale, it should recoil. We do not need to grip. We need to restore the natural rhythm of the core system. This improves circulation to the pelvic tissues. It promotes true functional strength.
The Role of the Practitioner: Signposting and Support
We are often the first line of defence. We see our clients weekly. We notice changes in their movement and mood. It is within our scope of practice to observe and listen. It is our duty to “signpost” or refer them to medical professionals.
We can suggest they speak to their doctor about their symptoms. We can mention resources like the Green Climacteric Scale. This is a symptom checker used by specialists. It helps women articulate what they are feeling.
We must also be informed about Hormone Replacement Therapy (HRT). The FDA has updated its stance on HRT. The “black box” warning has been removed from many products. For many women, HRT is a viable option for symptom management and bone protection. It is not our job to prescribe. It is our job to support our clients in finding the right medical care. We must be part of their integrated health team.
Further Information: Polestar Pilates Hour
For further information, in this recent Polestar Pilates Hour, Dr. Brent Anderson and Dr. Diedra Manns have an insightful conversation on supporting women through the physical, hormonal and performance shifts of perimenopause and post-menopause. Dr. Manns brings her expertise as a physical therapist and seasoned Pilates educator to explore how movement, nutrition, sleep, and stress regulation can improve well-being and resilience during this phase of life.
Click on the picture below and have a listen:
Conclusion
The future of Pilates lies in evidence-based practice. We must understand the physiology of our clients. We must recognise that menopause is a major physiological event. It requires specific movement strategies.
We have the tools to change lives. We can help women build resilience. We can help them maintain their independence. We can guide them toward a life of spontaneous zest and pleasure.
Are you ready to deepen your understanding of the human body? Do you want to master the assessment and critical reasoning skills necessary for this population?
Explore Advanced Continuing Education, View Course Dates, or Consult us to discuss your clinical application or career path. Let us help you become the expert your clients need.