The Science Behind Low Back Pathologies: A New Paradigm for Pilates
We remember a patient who came to us with a diagnosis of mechanical low back pain. He had been told by a well-meaning physician that his spine was “unstable” and that he needed to strengthen his core to protect it. This man was terrified to move. He walked stiffly, held his breath when he sat down, and had stopped playing with his children. His belief system was that his back was fragile.
When we looked at the science, however, the story changed. Research shows that 90% of adults will suffer low back pain at some point, and for many, it becomes chronic not because of tissue damage, but because of fear-avoidance behaviour and a lack of movement variety. At Polestar Pilates, we view low back pathologies through the lens of pathokinesiology – the study of how pathology impairs movement and, conversely, how movement can restore function.
The Myth of the “Weak Core” and the Reality of Load
For decades, the fitness and rehabilitation industries have been obsessed with “core stability.” The prevailing theory was that low back pain resulted from a weak Transversus Abdominis (TrA) or Multifidus. We were taught to cue clients to “hollow” their abdominals or pull their navel to their spine before moving.
Current research has dismantled this approach. Prof. Eyal Lederman DO, PhD, an osteopath and researcher, conducted a systematic review that revealed startling findings: weak trunk muscles are not a pathology but a normal variation, and core stability exercises are no more effective than other forms of exercise for preventing injury. In fact, constantly tensing the abdominals can increase compression on the lumbar spine and disrupt natural movement patterns.
Spontaneous vs. Volitional Control
The neuromuscular system is designed for efficiency. In healthy individuals, the core muscles fire spontaneously and subconsciously in anticipation of load. Studies by Paul W Hodges showed that the TrA contracts milliseconds before a limb moves to stabilise the spine – a reaction that happens faster than conscious thought.
When we teach clients to consciously grip their abdominals, we interfere with this natural timing. We create a “hypertonic” state where the muscles are tight but not functional. Instead of teaching clients to “brace” for every movement, we must create positive movement experiences where the body learns to organize itself naturally under graded load. The goal is not a rigid spine, but a spine that can distribute force dynamically across all segments.
Understanding the “Why”: Critical Reasoning in Pathology
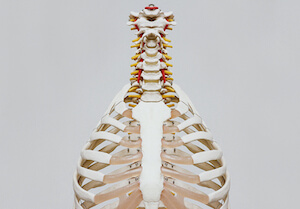
Low back pathologies are rarely just about the tissues. While we must understand the structural issues – such as disc herniations, stenosis, or spondylolisthesis – we must also look at the strategy the client uses to move.
Discogenic Pain and Flexion Intolerance
The intervertebral disc is robust, but it can become sensitised. In a healthy spine, the nucleus pulposus (the jelly-like centre) moves to distribute pressure. However, repetitive flexion under load can push the nucleus posteriorly, potentially irritating the nerve root.
For a client with an acute disc herniation, we might initially avoid loaded flexion to reduce sensitivity. But we don’t stop there. We look at why the lumbar spine is taking so much load. Often, we find a lack of mobility in the hips or thoracic spine. If the hips are tight, the lumbar spine compensates by flexing too much during activities like sitting or bending. By restoring hip mobility and teaching a proper hip hinge (a “deadlift” pattern), we spare the spine.
Stenosis and Extension Intolerance
Stenosis involves a narrowing of the spinal canal or foramina, often caused by bone spurs or facet hypertrophy. These clients typically suffer when standing or walking because extension narrows these spaces further.
The traditional approach might be to simply “avoid extension.” However, a pathokinesiologist asks: “How can we create length?” We use the Pilates environment to provide traction and support. By using the Trapeze Table or the Reformer, we can facilitate a lengthened spine that allows for safe movement without compression. We teach the client to find a “neutral zone” where the nerves have space to breathe, allowing them to walk and stand with less pain.
The Biopsychosocial Factor: Fear, Belief, and Neuroplasticity
Perhaps the most significant advancement in treating low back pathologies is the understanding of central sensitisation. Pain is an output of the brain, designed to protect us. In chronic cases, the “alarm system” becomes hypersensitive.
A client may feel severe pain not because of further tissue damage, but because their nervous system perceives a threat. Dr. Brent Anderson notes that psychosocial measurements – like fear of movement or catastrophising – are often greater predictors of outcome than physical measurements like strength or range of motion.
Shifting the Paradigm
As qualified Pilates teachers, we are in a unique position to change this narrative. We provide a safe environment where clients can move without fear. When a client successfully performs a movement they thought was impossible – like a supported squat or a gentle rotation – we invoke neuroplasticity. We rewrite the map in their brain that says “movement equals pain.”
We use graded load to build tissue tolerance. We start with assistance (using springs to support the weight of the limbs) and gradually progress to resistance. This process teaches the body that it is strong, resilient, and capable of healing.
The Polestar Approach
Treating low back pathologies requires more than a repertoire of exercises. It requires a deep understanding of anatomy, biomechanics, and the nervous system. It demands that we look at the whole person – their physical structure, their emotional state, and their lifestyle.
At Polestar, we train our teachers to be critical thinkers. We don’t just teach you what to teach; we teach you why you are teaching it. We equip you with the skills to assess movement strategies, identify red flags, and design customised programs that restore function and zest for life.
If you are ready to move beyond the basics and master the science of human movement, we invite you to join our community.
Pilates Hour #268 – The Science Behind Low Back Pathologies
Treating the Lumbar Spine and associated pathologies can be challenging at best. Watch and listen to this Pilates Hour where Dr. Brent Anderson PT, PhD, OCS, NCPT, explains a more profound look at the anatomy and pathologies associated with Low Back Pain.
Conclusion
Are you ready to deepen your understanding of low back pathologies? Do you want to master the assessment and critical reasoning skills necessary for this population?
Explore Advanced Continuing Education, View Course Dates, or Consult us to discuss your clinical application or career path. Let us help you become the expert your clients need.